>
| James (0:11) | Welcome to another podcast from the NIHR Health Tech Research Centre in Brain and Spinal Injury where I've been chatting to anybody with an interest in brain and spinal injury to tell me what they're doing at the moment and their thoughts about it. So I'm really pleased to be joined by Professor David Menon who is Director of Research at the University of Cambridge. Hi David, thanks for joining the call. | ||
| David (0:32) | Pleasure to be chatting with you James. | ||
| James (0:33) | And I wanted to get you on to talk a little bit about TBI Reporter which is a national project to pull together research about traumatic brain injury. How did that come about? | ||
| David (0:46) | We've been collaborating with researchers both in the UK, in Europe and in the US for some time and what became apparent to us as we ran through a whole series of studies is that we were doing these studies and at the end of the studies the bio samples and the data that was obtained from the studies were simply not used as much as we would like them to. And that's both economically illiterate because money has been spent on collecting that data. It's also scientifically undesirable because there's valuable information to be gained from it and it's also unethical because the data and samples come from families and patients who have provided consent for their research and we owe it to them to get as much information out of it.We need to make the squeeze worth the juice as the case as the Americans would say. So we have to get every last bit of information to do right by the patients who have consented to these studies. | ||
| James (1:44) | Yeah so what you're saying is someone's doing a project, they go out, they collect a load of information, maybe they do some samples, they publish their results but then there's more use we can get of the information they've collected. | ||
| David (1:55) | Absolutely and also there's information which you or there's insights that you can get by combining it. So for an example we know that outcome after traumatic brain injury is very variable and it's difficult for us to predict based on what they like clinically, how deep their level of unconsciousness is, what the scans look like and so on. We can predict about maybe 30-35 percent of the variance in outcome but two-thirds of the outcome is not predictable.The variance in outcome is not predictable. Now if we get blood biomarkers which are now emerging or we get MRI scans it gets up to 50 percent but still there's a large proportion of us not knowing why patients do as badly or as well as they do. So in an initial genetic study we demonstrated that the point prevalence, the best estimate we could have is about 25 percent of that variance was because of the person's genetics.
Now we did that in 5,000 patients which is a reasonable number but for a genetic study it really doesn't cut the mustard. Whereas if we could just collect the information from I don't know five or ten studies, suddenly we start getting up to the tens of thousands that allow us to identify not just what genetics are responsible for outcome but also those individual genetic variants. Why I might do better and someone else might do worse or the reverse provides us with targets that might allow us to develop new drugs. We really need to bring all of the information together and understand what it tells us. |
||
| James (3:27) | Yeah that's really interesting. Do we have any idea at the moment even this small study about which genes are involved? Are they related to anything else?Is it to do with ethnicity for example? | ||
| David (3:38) | So ethnic variation in genetics is much smaller than individual variation. What we know, what's emerging from it, as I said the sample size is relatively small, is that the way the body responds to the injury may be very important if you like what the person brings to the injury as opposed to what the injury brings to the patient. And their inflammation is starting to turn out to be a linchpin particularly one part of inflammation to do with complement and also whether the body produces if you like a vaccination response and produces antibodies against its own tissues.So there are some very interesting things that have emerged from our analysis and trying to pinpoint exactly what the mechanisms are there will allow us to think about devising new treatments. | ||
| James (4:25 ) | Yeah and then find new ways in. Okay so TBI Reporter itself isn't a research project then it's really just a repository to collect everybody else's research and combine that information. | ||
| David (4:37) | Yes and no. So TBI Reporter is not so much a study as a concept. So it's got four parts to it.A very key part of it is the patient and public involvement because we need to make sure that everything we do has the patient and their families at the centre of it. And we're very lucky to have, sparing your blushes, you and Chloe Hayward from UKABIF involved in this and leading the patient public involvement because that is at the heart of everything we want to do. The other three parts of it consists of a data hub and the data hub is where all of the information from past and ongoing studies would be banked if you like.
It'll still be under the control of the researcher who's collected that data but they can be they can have their data sets now discoverable which means that another researcher who wants to use that data can come along and ask for permission to use it. And if the ethical approval for that study allows such use of the data they can use it. And similarly we have a similar arrangement for bio samples and for imaging data and outcome data. Again with permission we can reuse the data. So this is being done as best as possible for retrospective studies, studies that have already been completed but as you can imagine often they don't have all of the information or not as much detail. But every new study going forward which is funded by a major UK funder will be asked to deposit data in TBI Reporter and bio samples in TBI Reporter. And so that means that we will be able to get the investment that's being made in those studies as a legacy for ongoing research. And that's a huge advantage. Now the final part of this is what's called an experimental medicine network. Over the last 20-30 years the pharmaceutical industry spent a huge amount several billions of dollars doing clinical trials looking at drugs that might be magic bullets in improving outcomes from traumatic brain injury. But all of them failed they showed no benefit. And what we have come to realise from a series of studies is that it may be because patients are very different, the disease may be very different in different patients. It's what we call precision medicine which means that we have to match diseases to treatments to the disease in individual patients. Now we're familiar with that for cancer. So for example if a woman is unfortunate enough to have breast cancer their breast cancer is typed so that we know what kinds of receptors and proteins they express or they show. And that allows the oncologist, the cancer doctor to pick specific treatments that are related to them. Now for us it may be much more related to what the person's response is. So if a patient has an excessive response to the injury produces a lot of inflammation they may wind up benefiting more from some of these treatments that damp down inflammation. On the other hand if they don't produce much inflammation and you damp down inflammation they may have a very high risk of getting things like secondary infections or pneumonias and so on. So there's a matching of treatments to patients that allows us to do it. So we want a whole new series of studies but the pharmaceutical industry is very very wary because they've had their fingers burned. What the experimental medicine study allows us to do is to take very small numbers of patients and instead of looking to see whether it makes a difference to the eventual outcome which typically requires a couple of thousand patients in severe brain injury we can ask does it do anything to the mechanisms that we know are important. And if it makes a difference to the mechanism then there is every likelihood that it's going to be beneficial and we could then take it into a large trial. So those early stage trials allow us to fail soon which is just as important because we don't want to be subjecting patients to trials of ineffective therapies or succeed rapidly in deciding which treatments we take forward for larger and more definitive trials. And we have a network of centres that have the ability to do slightly more complicated studies than the average trial so that we can look at all these mechanisms and see how new drugs or for that matter old drugs will interfere with those. |
||
| James (9:08) | Yeah and then I guess the aim is to tie that into the genetic things you were talking about before maybe that variance relates. So when I turn up with my brain injury I'm assessed yes you're suitable for that treatment and you're suitable for that treatment and we get a bit more kind of personalised approach. | ||
| David (9:26) | Absolutely. So we haven't reaped the benefits of this outside cancer medicine as well as we should but for a whole range of diseases we're starting to realise that this might be helpful and now for the first time we have small tabletop instruments we can put a single blood sample into and get the information back about either the levels of the chemicals or the genetics within a few hours. So it's within the time window when you can have early treatments that make a difference to patients outcomes. | ||
| James (9:55) | Yeah and make a change. Fantastic. So TBI Reporter is collecting this information now.Studies that have already finished are depositing their data in the system and are we starting to see some results of people interrogating each other's data already? | ||
| David (10:10) | The first study that we've now done is based on data that's obtained from a large ICU registry of traumatic brain injury and that has shown that the incidence of mortality has been going rapidly up in patients who are suffering from traumatic brain injury and it's been going up at a more rapid rate than you would see for other causes of trauma or other causes of brain injuries such as strokes and other critical illnesses such as people who come in with sepsis and one of the reasons is that patients are often having treatment withdrawn at relatively early time points because it's thought that their outcome is going to be so bad. Now that may be entirely appropriate but highlighting that means that we have to look at it carefully and make sure that doctors and intensive care units are not being unduly pessimistic and that's something which we will address over the next year or two years but it's also shown that the incidence of low levels of oxygen and low levels of blood pressure in the early phase after severe brain injury has become much more common and we ask ourselves why that is the case and there are two possibilities. One is that we now have a major trauma system across the United Kingdom and it means that we are getting in patients are so sick that they would have died at the roadside before so it may just be that the patients are sicker but there's also a recognition that keeping the blood pressure very high or giving very high levels of oxygen for other causes of critical illness other causes in patients who are very sick can be harmful in its own right and maybe people have rolled back a bit but maybe the pendulum has swung too far in the other direction and maybe for patients who have primary brain injury we should allow slightly higher blood pressures and particularly slightly higher oxygen levels than would be optimal if they didn't have brain injury if the primary problem was that they had an infection from a ruptured bowel or something like that. | ||
| James (12:14) | Yeah and I guess both of those things are really sort of before people get to hospital right so you're scraped off the road and the treatment you get in those early stages more people are surviving to get to hospital because it's good but it's also another place where we perhaps need to target the treatments and identify quite quickly if people have got traumatic brain injury and perhaps then handle them slightly differently before they go to where they need to be | ||
| David (12:39) | Absolutely and the thing about these changes are they don't require a new treatment what it requires is a subsequent study that tests this hypothesis that we should be putting up the oxygen levels or we know that the associations are there so we would just modify the guidelines or educate pre-hospital doctors and doctors in emergency departments a little bit more and say well don't let the oxygen levels get we're not asking them to keep the oxygen levels very high but say in patients who may or are known to have a brain injury we should keep the oxygen levels just that bit higher than we would if people came in with another pathology. Typically you and I would run oxygen levels of 95, 96, 97, 98 percent if you've got healthy body typically 97 or 98 percent. What we've realised is that allowing patients who have other diseases to get their oxygen saturations up to 100 percent is probably harmful and running them at maybe 92 percent is just as good if not better but in patients with brain injury there's a case I think based on a lot of circumstantial evidence though not a formal trial that keeping the oxygen saturation levels at 96, 97 percent may be more favourable than letting it drop to 92 percent and that's easy to do but the health tech research centre has also pioneered and we're testing instruments that look at oxygen levels in the brain itself and that may provide us with a more direct way of looking at the brain. So let's go away from oxygen levels to blood pressures now supposing someone comes with multiple trauma and they've ruptured the aorta the big blood vessel in their tummy and that's leaking a bit. Now under those circumstances you don't want the blood pressure to go very high because that leak would become catastrophic but at the same time if they've had a brain injury you want to make sure there's enough blood getting to the brain so being able to measure blood supply in the brain with something non-invasive a little helmet that gets plopped on the head means that you can titrate it very carefully get the blood pressure high enough so that you're getting enough blood supply to the brain but not so high that you're going to increase the risk of leak or you minimise the risk of leak as much as you can under those circumstances and you may not be able to get the best solution because the best solution for one injury may be one thing and the best solution for another injury may be another thing but you'll certainly be able to arrive at the least worst solution and that I think is something that we're looking forward to. | ||
| James (15:08) | Yeah interesting certainly there's a couple of projects that we've been talking to recently trying to measure intracranial pressure non-invasively and blood flow and oxygenation and so on so yeah really interesting ripe areas for research. So are there new pieces of research that are feeding into TBI Reporter that we know of? I guess there's a whole range of groups all across the country who are doing stuff in this area and hopefully kind of feeding in to Reporter. | ||
| David (15:33) | Yeah so it's probably best to look at it in three areas in looking at diagnostics and looking at new treatments and then in rehabilitation. So for diagnostics there's a huge interest now in looking at blood biomarkers these are proteins that are released by the brain when it's injured and there's now a lot of technology which is approved by the FDA in the USA and the CEA in Europe which tells you about whether the brain's going to be so badly injured that you should be you should always get a CAT scan of the brain or whether it's so low that the radiation burden of a CAT scan is undesirable. It isn't quite being realised how that would fit into our clinical practise. The NHS does things in a very orderly way and we have guidelines for when patients get CAT scans.So Virginia Newcombe and Fiona Lecky are running a study looking at these biomarkers in UK clinical practise not just looking at the efficacy and whether they can give you a better answer but whether this is cost effective because we want to make sure that we have the best bang for our buck. So that's an example of getting better diagnostics. | ||
| James (16:44) | Yeah and I guess potentially there there's cost savings because if we're scanning people who don't show anything on the scan and we're wasting our time and we're not doing that aren't we. | ||
| David (16:54) | And also savings in radiation burden particularly for younger people the increased risks associated with a CAT scan of the brain are relatively small but it's not worth having that if you don't need it and also it may tell us patients in which the CAT scan looks normal but where you should do an MRI and both at both ends of the spectrum very mild traumatic brain injury or very severe traumatic brain injury we've shown that biomarkers can tell us which patients should have an MRI.So that's diagnostics but then if you go to treatment I was talking to you about the response that the body makes in terms of inflammation and we have a lot of experience from COVID as it turns out in using drugs that reduce inflammation and one of those is a drug called tocilizumab which reduces the inflammatory processes that the body mounts against any kind of injury or any kind of infection. And we know from COVID that the drug is relatively safe even in particularly in patients and Edward Needham was one of the people in Cambridge is running a clinical trial using the experimental medicine paradigm that I talked about looking in small numbers of whether it changes the processes of disease and using tocilizumab there and that will tell us whether we need to mount a larger study and it might make a big difference and just like we talked before we may find because we'll be looking for it that it's effective in a subset of patients and we'd be able to target those patients in a bigger trial. And then finally there's a lot of work to be done in terms of rehabilitation and one of the first steps for that is to understand what the outcomes are after traumatic brain injury or the trajectory of recovery is and one of the one of the things that we have on the platform is a measure of outcomes that have been devised by Adam Hampshire from King's and we'll be able to collect all of this information online making it easier for patients to enter that information and then once we've got the trajectory we can start asking how we change those trajectories with interventions.
So there's a lot of very exciting developments now. |
||
| James (18:58) | TBI Reporter has been running for a couple of years now how much longer do we see this something that's going to be in 20 years time still collecting data and sharing it? | ||
| David (19:05) | We hope so we have another three years of funding and we have some backup funding for two years after that but as we get to the end of the five years probably in the fourth year we'll be asking for money to keep it running for another five years. We had a very large initial grant and I should say thank you to the funders because they showed a lot of foresight and these include the National Institute for Health Research, UK Research and Innovation in the form of the Medical Research Council who are the lead funders for this, the Ministry of Defence because traumatic brain injury is a big problem in civilian traumatic brain injury is a big problem for the for the Ministry of Defence and the military and finally Alzheimer's Research UK and I would particularly like to highlight their foresight because we know that traumatic brain injury is one of the modifiable risk factors for late life dementia and by putting money into this they have recognised this important fact and we may be able to look at really long-term outcomes because we can link data across the NHS. So we will apply for ongoing funding but we will find one way or another of keeping this going it's too important not to do so. | ||
| James (20:21) | Yeah and well hopefully the thing that will swing that is that we start to show some changes right we have some learning and maybe it's about that kind of personalisation that you spoke about. | ||
| David (20:31) | Correct and also it's important to say that through the patient public involvement and engagement and through UKABIF we've been able to engage with the all-party parliamentary group on acquired brain injury so anything that we find even if it's a simple solution we can take to the policymakers and not just educate ourselves as clinicians but also educate the policymakers and make sure that measures for prevention and measures for treatment can be incorporated into national policy and there's a useful example of that. One of our collaborators is the transport research laboratory which collects data from every road crash and that is amazing because so far we've looked at the disease very carefully but we haven't been able to look at the dose of the pathogen the dose of the insult.Now we can start getting lots of information about why the crash happened how severe the crash was and we can start making changes to how cars are, improve their safety so there's there's a connection here that suddenly becomes very exciting so that could feed into policy as well. | ||
| James (21:41) | Yeah because of course the very best treatment for traumatic brain injury is not to have one in that public health messaging. Well David thank you ever so much for joining me on the podcast and sharing some story about this I'll put a link to the TBI reporter website underneath this podcast and check it out and remember listen to other episodes in this series subscribe like do the thing that young people do all the time and thanks. |
More like this:
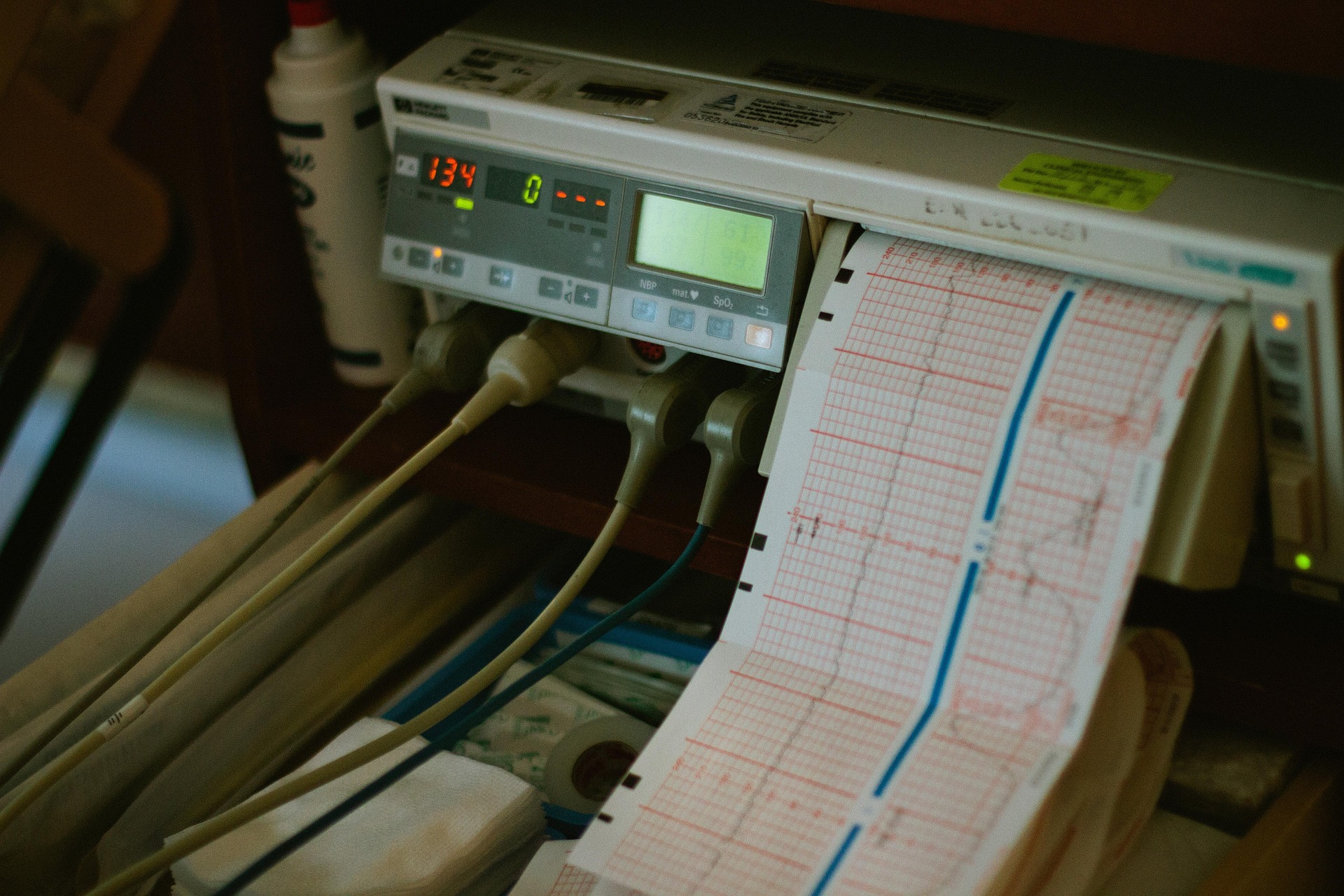
Innovation Podcast – Fetal Monitoring
James talks to Antoniya Georgieva of Oxford University about fetal monitoring and the use of AI to [...]
Paper on PPI in brain injury research
James, our PPIE lead, has written a paper outlining the development of our outreach programme over the [...]
Innovation Podcast – Eye Focus
James talks to Stephanie Rossit about spatial neglect and a new app designed to help the many [...]