Listen to our Diagnostics Theme Lead, Professor Stephen Price, talk with James Piercy about our diagnostics theme.
Stephen and James discuss new techniques for understanding how to diagnose patients correctly, some of the limitations of current diagnostic practice, and the importance of diversifying data across different injuries, communities and ethnic backgrounds. How can we strengthen the prognosis for patients by looking at the data we collect and changing the current pathways in place?
| (0:09) James | I'm talking to Stephen Price and Stephen is one of the Theme Leads for the HealthTech Research Centre in Brain and Spine Injury. And Stephen, it's the diagnostics theme that you are leading. Can you tell us a little bit about what that theme is for, what are we hoping to find out and develop? |
| (0:26) Stephen | So, diagnostics is a thing that we need, a step that we often don't have a lot of tools to help us with. So it's not only just diagnosing conditions, but it's also more than that, it's also giving us information about how we might want to treat an individual patient. And providing information about how a disease, process, or recovery might happen in an individual patient. So, there's lots of things for it that we can be dealing with, and it covers a whole multitude of things, from sort of handheld devices that might provide some diagnostic information, through to imaging techniques, through to techniques that we can now do on blood, urine. Through to things that use machine learning and artificial intelligence as well, to help us interpret information to make a diagnosis. |
| (1:20) James | Okay, so a whole range of things and obviously depending on the condition that we're dealing with we're going to use different techniques. Why don't you give us an example, so if somebody is suspected of having a tumour, what kind of equipment would be used at the moment to diagnose that? You need to find out how big it is, where it is, I guess; what sort of things would be used? |
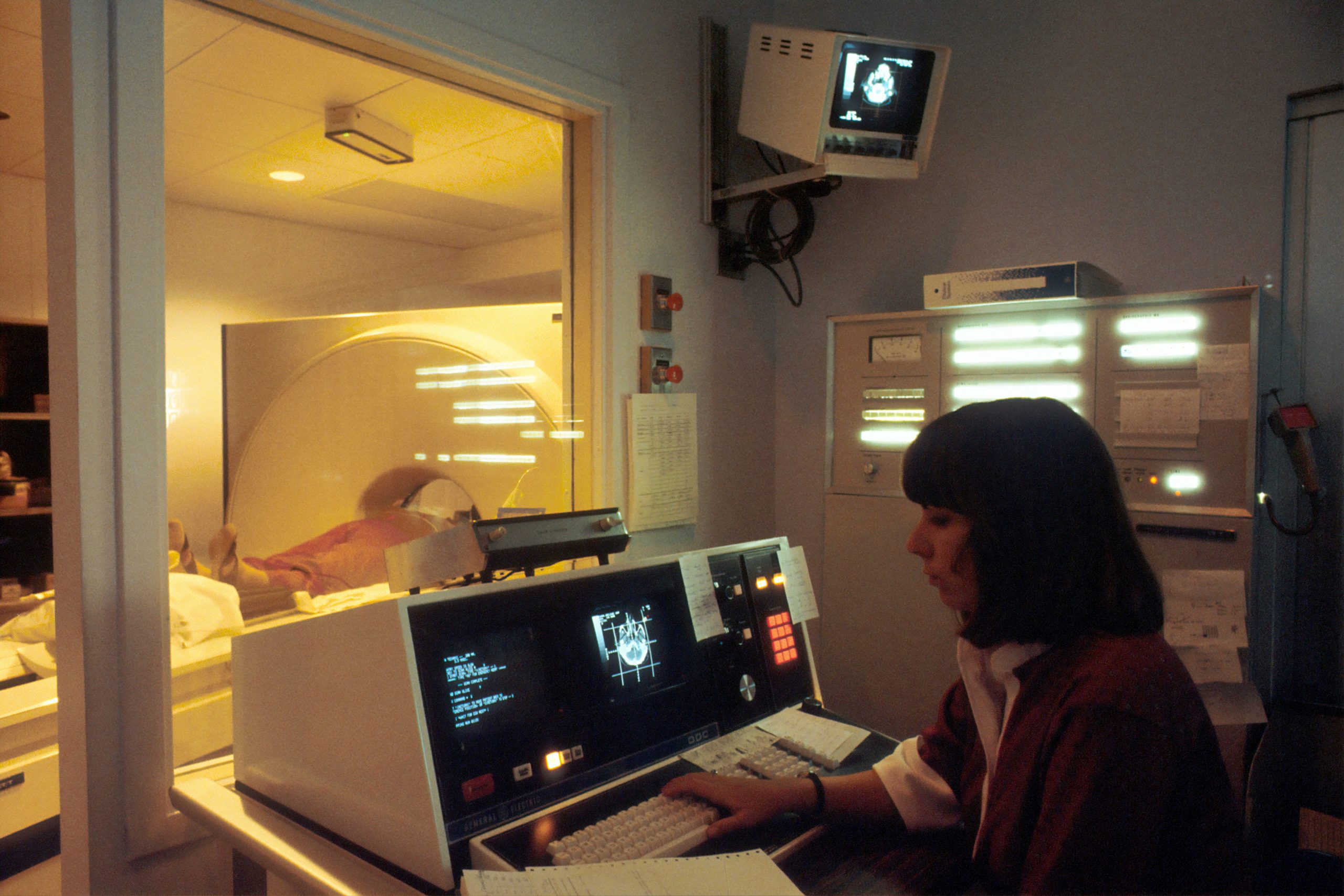
| (1:41) Stephen | My main area is tumours and operating on patients with brain tumours. And we will use MRI scans on all patients, all our patients will get an MRI scan before surgery. And the idea is whether we can tell more information than you can get from the MRI scanner. So, could we, for example, tell you exactly what the diagnosis is? Could we tell you some of the changes that have occurred that have led to this, that might allow us to, sort of, tell us which treatments might have a better effect in certain patients? And also give us some information about prognosis. Is this something which is going to be a better prognosis or a worse prognosis, that we can have quite detailed discussion with the patients before we embark on treating it to think of what's the best way of treating this for that individual patient? |
| (2:30) James | Yeah, and I guess there's always this element of patient choice, isn't there? In these cases, some people might be deciding, do they have surgery or not? Do they have some other kind of treatment or not? And as you say, getting that idea of prognosis is really important there. |
| (2:45) Stephen | Absolutely! And also a bit about, what kind of treatment do you have? Whether you go for something which is more aggressive treatment, which may have better longer-term outcomes, but is higher risk for the patient, right at the beginning, of developing more injuries to the brain, and having more problems from it. Or whether you have something which is not as aggressive, so you're not having the problems of developing injuries to the brain, but also it may not be enough so that the tumours are going to come back at a much shorter interval. And it's those discussions are actually really difficult for us to have. So having something that could give us an idea, some sort of diagnosis, tells us a little bit about what's going on with these patients would be a really helpful thing for us to have. |
| (3:32) James | Yeah, interesting! And so what about a different case? What if there's been a traumatic brain injury, someone's had a bang on the head? Again, there we need to get some idea of exactly what's happened to the brain and some kind of idea of what might happen in the future. Do we use similar technologies at the moment to do that? |
| (3:49) Stephen | So again, MRI scans are used for that, but there's also the opportunity for having some sort of scanning device that could provide information very early on, as whether there's a blood clot there, to work out whether the ambulance crew takes a patient to a neurosurgical unit, which may be a longer journey, or just to the nearest emergency hospital. So, there are some things around that. There are also, one area that there's a lot of interest in, in terms of traumatic brain injuries, in sports concussions, sports injuries. So you see sort of rugby players or involved in tackles, and you see a lot of them afterwards acting a bit confused. Well, the infield testing things aren't great, and they're very hard to do. If you could have a chemical that you could detect (and some people are doing this from saliva, some people are doing this from tears) that you could get some chemical and just see whether or not that had been increased, which tells us that there's been a significant injury to the brain. It would be a really big leap forward for us to be able to use for these patients, and tell us within a short period of time whether that person should go back onto the field or not. |
| (4:56) James | Yeah, interesting. So we call those biomarkers, don't we, these sort of chemical signals. Are they always things that are produced after an injury, or perhaps will we see something that decreases because of an injury? |
| (5:08) Stephen | You can probably get a bit of both. Most of the biomarkers we look at are things that are produced, so there's something you can detect and identify. It's often harder to detect a lack of something, rather than to detect something present. And that's why we often look for things that are there. Because if they're not present, it may just be because the test hasn't worked. But it's much better that we find something that we can use, to tell us that there is definitely a positive change within that person. |
| (5:41) James | And how quickly are those materials produced in the brain? Is it within seconds of injury? Minutes, hours? |
| (5:48) Stephen | All of the above! So, there will be some that will have a very acute presence, that we see very early on. There'll be others that then come on a bit later on, and tell us a bit more about the latter part of things. And others will appear much later on, even into the recovery phase. What most of the work is focused on at the moment, is those ones you see right at the very beginning, because most of the work on this has been done around the whole area of triaging patients who've had a head injury, with what sort of treatment they should go and have. |
| (6:16) James | Yeah, and where to send them. And I guess the other thing is, you might have a CT scan or something which doesn't really show anything. But we know that lots of those people actually have quite long-term impairments and suffer quite badly. So is there a chance that these biomarkers could predict that? You probably don't need to come into hospital, but watch out for X, Y, Z. |
| (6:36) Stephen | Yeah. Yeah. So that's what we're hoping for. Is that, being able to identify patients who have got a significant injury. Because you're right, the CT scan often doesn't show (in fact, even often MRI scans show) very little. And patients can have quite profound problems and symptoms from head injuries. And then working out, who can we say: look, this is going to be fine; And who do we say, actually, we need to keep an eye on you, and just think about patients who might be suitable things like a rehabilitation program. |
| (7:05) James | Excellent. So are all of these diagnostics technologies, do you think, about taking pictures or taking samples from people after injury? Are there other kind of diagnostic techniques that might think about the patient's baseline, their pre-morbid state? Are there kind of any investigation to that? Because we know that they have a huge impact on outcome after brain injury. |
| (7:25) Stephen | Yeah, so, some work has been done on this, mostly in the Alzheimer's field. But there is a thought about whether it can be transferred to other areas. And it's a thing called cognitive reserve. This explains why you can find patients who have got a scan of their brain, which looks pretty much normal, but have got severe dementia. Whereas other times you come across (and this is a very much a Cambridge thing), you find these professors of this and that in their 80s and 90s, who have an MRI scan, which shows a brain that is really shrunken down, but they're as bright as anything. And it's understanding why some people will get problems with this and why others won't. And this is particularly important for looking at the longer-term outcomes for various diseases, because it's the same sort of principle. So we know, for example, after head injury, you lose some of the neurons, the nerve cells within the brain, and that can lead to dementia later, much, much later on in life, and whether you could identify those patients at a much earlier stage. So there is a bit of work around that. And that's often assessed with questionnaires. So there are certain questionnaires that have been validated, that can actually provide this sort of diagnostic information about patients, and give you an idea of what their baseline might be. |
| (8:44) James | Yeah, interesting. So that sort of suggests that, as with dementia, if we learn more, we might have better recovery from other kinds of brain injury as well. |
| (8:53) Stephen | Yeah, I think that's the case. Is having a better understanding of who is going to respond better from rehabilitation and, in the longer term, sort of having these ideas. And some of that comes from basic information that we have before the injury. |
| (9:10) James | So you mentioned imaging MRI and we touched on sort of CT. Are there improvements in those technologies coming through? Because those scanners are really common now in hospitals, aren't they? Are they getting better? Are they getting more powerful? |
| (9:23) Stephen | Yeah, they're getting better, they're getting more powerful, and they're getting faster. And the beauty of them being faster, means that you can also then start doing, what is now called, multi parametric imaging. And what that means is you can then start doing special imaging techniques, that tell you a little bit about what the pathology is going on there. So not just what it looks like, but actually more about what goes on there. What's the blood flow like, for example. The cables of the brain, how are they doing and how are they disrupted by whatever the condition is? And these are simple techniques that can be done on any modern scanner. They're often not done because they take time, or there's no one there with a specific interest to actually better interpret them. The other big issue, and this is one of the really key things for our theme, is that, so, for example, a lot of the work on these advanced MRI techniques that tell you a bit about pathology have come around in my field in brain chambers. Yet if you look at it and say, how many do we use on a regular basis, the answer is virtually none of them. And the reason for that is: no one's done the study that has shown it changes your management. And this is one of the key things about a diagnostic is that - it's all well and good saying that it tells you about something - but you've got to go to the next stage and show you that, actually with that information, you change what you're going to do for that patient, or it changes somehow how you will manage that patient. And that is missing, that's completely missing from the field. So our concept, is trying to work out a pathway, that we can take a diagnostic (and pretty much independent of what it is, it doesn't matter whether it's a tissue sample or a bit of a urine test or a blood test or whatever) and take that, and provide a pathway, of how you might develop that pathway. From having a nice idea about this; through to testing it, to see whether it actually tells you what you think it tells you; to the next stage of actually, then, showing that it makes a difference to your management, and with all the cost effectiveness information that you need for it. All the way through to, effectively, going before the National Institute of Clinical Health and Excellence to say, “Yes, this is a thing that needs to be used in patients on a regular basis.” |
| (11:35) James | Yeah. And I guess what we need to do is to publish a load of research so that when they do the clinical guideline reviews, then take those papers, and build up an evidence of cost effectiveness to show these new things work. |
| (11:47) Stephen | One of the big issues about diagnostics is it unlike, for example, if you've got a new treatment. So, you've got a new treatment and you want to give it to patients. It's very easy. We know exactly how to run these studies. You have these randomized studies where some patients get it, some patients don't get it, and you then compare how the two groups get on. Diagnostics is more complex than that because, not only do you have to look at whether or not you can detect disease, for example, in a patient group or not – accurately; but also how does the test perform? So, if I was to do the test on a single patient and did it four times in a row, would I get the same results from it? And that is an important thing that has to be factored into this, as part of our discussion. One of the areas that is, at the moment, a real talking area in the field of diagnostics (this is particularly the case where we use artificial intelligence to help us interpret the results of this) is how accurate a result is enough. Because all clinicians will say, oh, 100 percent accuracy. You can't get that, that's just impossible, you'll never have that test. Is 90 percent good enough? Is 85 percent good enough? Is 75 percent good enough? And that's the difficult thing we need to think about as well is, what would people accept? And this is (I think) where the PPI part of it really comes into itself, is that we need the public really to tell us, “well, I'd be happy if I had a test that would tell me with 75 percent confidence that this” or “85 percent confidence”, and give us an idea of what we need to do for our testings. |
| (13:29) James | Yeah, and where those sort of lines are. And I guess one of the other problems is that we don't have anything that's perfect, at the moment. Normally, what you do is compare a new thing to the gold standard, which is always right. But we don't have anything that's always right. The thing you've got might be better than the thing you're comparing against. So, there's that kind of challenge. You talked a little bit about artificial intelligence and machine learning. For those systems to work, they just need loads of information, don't they? Loads of data. So, does that mean to start with, you just run these new tests alongside the normal procedure and you're just harvesting data, really, rather than changing anything about the treatment of those patients? |
| (14:04) Stephen | Yeah, getting the data for this is a real issue within the field. And it's difficult to know the best way of doing it. What we would love to have, is access to anonymized data that we have in the NHS. The NHS is a great system because we can get all this data very easily. And it would be great if we had the permission from patients, we just use their data anonymously, to train these machine learning techniques, or these artificial intelligence techniques, so that it can start detecting these changes. Traditionally, what we've done is we've just tried to collect as much data as we can and see if we can train on that. There are a lot of publicly available data sets in certain areas, but only in very specific areas. So again, in my field of brain tumors, there's a big set on the malignant brain tumors. There's not a lot on the benign brain tumors. So it's very hard to develop a diagnostic, or a machine learning technique, that can interpret what's going on in that group of patients, because you just haven't got the numbers to do it. And certainly, the more you have, the better accuracy of your technique. |
| (15:13) James | I guess the other thing I want to pick up with the machine learning thing is there's always this risk of bias, isn't there? That, the people that are providing the data are all the same, so we end up with a really reliable result for white Western men. But, actually, it doesn't necessarily apply for other groups, so are there ways around that? We just need to track whose data we're collecting? |
| (15:33) Stephen | Yeah, this is so important, and it's been such a mistake that people have made over the years. For example, a lot of the automatic software that was used to detect malignant melanomas (or skin cancer, where you get these sorts of dark moles within the skin) was done on white skin. So, of course, if you've got someone with darker skin, it doesn't work. It is so important, we need to make sure that our data set comes from the population of people that have this disease, across the whole population. And we can see the differences between different groups. And we just have to be very careful, making sure that we look at who we have the data from (to make sure there's a good mixture of data), but also make sure we look for sources of data that can actually allow us to get across the whole field. And it's so important that we make sure that we don't make it so it only detects for certain people, and it will work on everyone. |
| (16:33) James | Yeah, definitely. And I'll put in a little plug here for the RHITE database. Because we also want the patient and public involvement from people from all different communities and all different backgrounds. If people listening to this are interested in becoming involved, and supporting development research projects, you can sign up to the RHITE database. There'll be a link underneath this very podcast. |
| (16:52) Stephen | It is so, so, important that we have this input. And as we said, it's essential that it's all types of people just so we get a proper cross-representation of things for our studies. |
| (17:06) James | Great. Well, thanks ever so much for your time, Stephen. It was great talking to you. And we look forward to seeing more developments in the diagnostics theme. |
| (17:13) Stephen | Thanks. |
More like this:
Innovation Podcast – Crainio
Listen to James Piercy talk with Jeremy Holland, Chief Executive of Crainio, about their non-invasive intracranial pressure [...]
Research Podcast – Matthew Colbeck
Listen to James Piercy talk with researcher Matthew Colbeck Matthew's work explores the ways that coma and [...]
Patient Involvement Podcast – Greg Dean
Listen to James Piercy talk with Greg Dean, member of the HRC public oversight committee Greg's life [...]